Data-Driven Approach Successfully Engages Orthopedic Surgeons in Decreasing Opioid Use

- 35 percent relative reduction in the total number of opioid pills prescribed.
- 20.4 percent relative reduction in the average number of opioid pills per prescription.
- 239,230 fewer opioid pills available in the community.
The U.S. is facing an opioid epidemic and outpaces all other nations in opioid prescribing for hydrocodone. Orthopedic surgeons are the third-highest prescribers of opioids, and when compared to prescribing patterns of other countries, underuse non-opioid alternatives for pain management.
Community Health Network (CHNw) was keenly aware of the impact that opioid prescribing patterns have on potential opioid misuse and set a focus on decreasing opioid prescriptions; however, it lacked access to meaningful data that could be used to understand the volume of opioids that were prescribed postoperatively. Without further information, providers were reluctant to change their prescribing patterns.
To address this challenge, CHNw created an orthopedics guidance team and leveraged data within its analytics platform to gain insight into prescribing habits over time, including the most frequently prescribed medication and the volume of pills prescribed by individual providers. This data drove peer-to-peer conversations among providers and discussions with patients related to reducing opioid use.
POTENTIAL FOR OPIOID MISUSE RAISES CONCERNS
Since 1999, the U.S. has experienced a steady increase in deaths from drug overdose with an average of 130 Americans dying every day from an opioid overdose. In 2017 alone, there were over 70,000 overdose deaths, 68 percent involving an opioid.1
In Indiana, providers wrote approximately 5.8 million opioid prescriptions during 2015. The following year, there were 794 opioid-related overdose deaths in the state—a rate of 12.6 deaths per 100,000 persons compared to the national rate of 13.3 deaths per 100,000 persons.2 The U.S. outpaces all other nations in opioid prescribing for hydrocodone. Orthopedic surgeons are the third-highest prescribers of opioid prescriptions and use fewer non-opioid alternatives than other countries.3
The quantity of opioid pills prescribed after surgery is a predictor for the quantity consumed by the patient. Also, only about 27 percent of opioids prescribed postoperatively are consumed by the patient, leaving unused opioids in the community, increasing the risk of opioid misuse and addiction.4
Community Health Network (CHNw) is a non-profit healthcare organization serving central Indiana, ranking among the nation’s most integrated healthcare systems. Based in Indianapolis, it strives to improve health and well-being in the communities that it serves, providing convenient access to exceptional healthcare services, where and when patients need them—in hospitals, health pavilions, and doctor’s offices, as well as workplaces, schools, and homes. CHNw needed to fully understand the opioid prescribing patterns of its providers to properly serve its community.
LACK OF DATA HINDERS UNDERSTANDING OF PRESCRIBING PATTERNS
While participating in an international mission trip, the CHNw orthopedic service line leader noted that the patients for whom he was providing care in other countries received far less postoperative opioids, often managing postoperative pain with nonsteroidal anti-inflammatory drugs and forgoing opioids entirely. Returning to the U.S., he conducted a deep dive into his personal prescribing patterns and was surprised by the volume of opioid medications prescribed in one year.
The service line leader and other orthopedic providers at CHNw were keenly aware of the impact of opioid prescribing patterns on potential opioid misuse. While conscious of the potential negative effects, the providers did not have access to meaningful data about their prescribing patterns and how those prescribing practices compared to their peers. Further, providers relied primarily on practices learned during their initial training and were often unaware of new state and federal opioid prescribing requirements.
Without data demonstrating the need to change, providers hesitated to alter long-held prescribing patterns. They were concerned about receiving additional refill requests, finding the time required during clinic visits to discuss pain management alternatives to opioids, and potential negative impacts on the patient experience, particularly since patient experience scores were previously tied to the providers’ variable rate compensation plans.
The orthopedic service line wanted to address the opioid epidemic, but providers lacked the ability to monitor their prescribing habits effectively, and could not analyze appropriate or inappropriate trends. To make lasting practice changes, CHNw needed better data.
DATA-DRIVEN APPROACH FACILITATES EFFORT FOR DECREASING OPIOID PRESCRIPTIONS
CHNw holds a vision for quality, aiming to deliver an exceptional experience to every life it touches. The organization has a robust improvement approach used across the network focused on improving quality as defined by its individual patients, based upon outcomes, experience, cost, and the appropriateness of care.
Establishing an orthopedic guidance team
To achieve its vision of quality, CHNw has invested in permanent improvement teams. One such team is the orthopedic guidance team, responsible for facilitating progress within the orthopedic service line. This team identified opioid prescription reductions as a top priority, initially focusing its improvement efforts on reducing the number of opioids prescribed at discharge following orthopedic surgical procedures.
The orthopedic guidance team established a goal of an 18 percent relative reduction in the average number of opioids per prescription. Understanding the importance of actionable, timely data to engage providers in change, the team also created a goal to implement robust analytic capabilities, including visualization of performance that could be used to inform providers of their individual prescribing patterns and habits.
Incorporating analytics to gain insight into prescribing practices
To extract and integrate data from many source systems, CHNw relies on the Health Catalyst® Data Operating System (DOS™) platform. Leveraging data within the analytics platform, CHNw developed an Opioid Analytics Application to gain insight into prescribing habits over time, including the most frequently prescribed medication and the volume of pills prescribed by individual providers (see Figure 1).
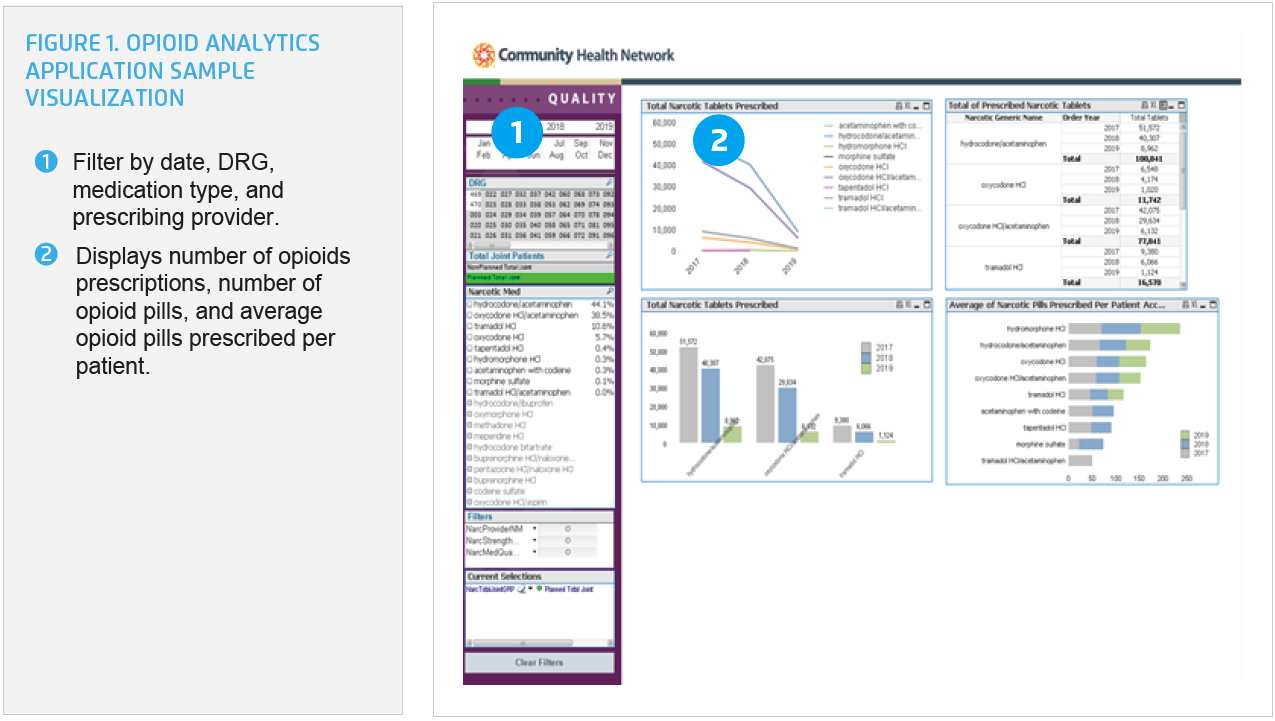
For the first time, CHNw has near real-time orthopedic opioid data. The analytics application supports users in drilling down to individual provider, patient, surgical procedure, and type of opioid prescribed. Data analysts are able to make comparisons of opioid prescriptions over time to understand differences in prescribing patterns.
The analytics application supports users in drilling down to individual provider, patient, surgical procedure, and type of opioid prescribed. Data analysts are able to make comparisons of opioid prescriptions over time to understand differences in prescribing patterns.
Data spurs conversations with providers and patients
Using the data gained from the analytics application, the service line leader began discussions with each provider in the practices, sharing each individual’s opioid prescribing data, and sharing how their prescribing practices compared to that of their peers. The service line leader also shared examples of the small tests of change he had made in his own prescribing practices, and was able to demonstrate that there was not a negative impact on the patient experience, conversations with patients did not take an exorbitant amount of time, and had not increased the number of patient calls after discharge.
These personalized peer-to-peer discussions explored how the provider compared to their peers, national trends in opioid prescribing, and offered an opportunity to talk about concerns. CHNw also made education available to providers to help them better understand the state and federal limits on the number and frequency of opioid medications that can be dispensed at one time.
Changing prescribing practices required that providers engage their patients in a dialogue regarding the risks of opioids, the need to increase the use of non-opioid pain management strategies, and the importance of reducing the number of opioids prescribed. To support providers in having these discussions, CHNw shared best practices, including scripting, that providers can use to guide their conversations with patients and families.
Clinic support staff were provided education and empowered to begin conversations with patients and families during pre-surgery clinic visits for expectation setting about postoperative pain, strategies to manage pain other than by opioid prescriptions, and the importance of limiting excessive opioid pills in the community.
Public awareness of the risks of opioid prescriptions contributed to patient and family interest in the topic and increased their willingness to utilize non-opioid pain management treatment options. In addition to one-on-one peer education, CHNw shares unblinded opioid prescription data at quarterly service line meetings. Transparent data sharing allows providers to continue to evaluate their performance in relation to their peers.
RESULTS
Using this data-driven approach to engage providers in changing opioid prescribing patterns, CHNw has realized substantial progress in decreasing opioid prescriptions, including:
- 35 percent relative reduction in the total number of opioid pills prescribed, outpacing the 18 percent goal.
- 20.4 percent relative reduction in the average number of opioid pills per prescription.
- 18.8 percent relative reduction in the number of opioid prescriptions.
- These reductions resulted in 239,230 fewer opioid pills available in the community, decreasing the potential for opioid misuse.
- Maintained patient satisfaction with pain control.
“Along with holding data and analytics to demonstrate the issue, having a shared group goal and increasing conversations has empowered physicians to reduce opioid prescriptions.”
– Stephen Sexson, MD
Orthopedic Surgeon
Network Product Line Leader
WHAT’S NEXT
Building on the success of the orthopedic service line, CHNw plans to establish standard prescribing guidelines for each surgical procedure. Additionally, the improvement team is engaging the anesthesiology group to collaborate on opioid use reduction strategies during the inpatient phase of orthopedic surgeries and is planning on expanding the team’s work systemwide, engaging more service lines to ensure patients receive adequate pain relief while also minimizing the risk of opioid misuse.
REFERENCES
- Centers for Disease Control and Prevention. (2018). Opioid overdose – Understanding the epidemic.
- National Institute on Drug Abuse. (2018). Indiana opioid summary – Opioid-related overdose deaths.
- Morris, B. J. & Mir, H. R. (2015). The opioid epidemic: Impact on orthopaedic surgery. Journal of the American Academy of Orthopaedic Surgeons, 23(5), 267-271.
- Rodriguez, A. (2018). Patterns of prescribed opioid use after surgery linked to prescription size, study says. The American Journal of Managed Care.
This website stores data such as cookies to enable essential site functionality, as well as marketing, personalization, and analytics. By remaining on this website you indicate your consent. For more information please visit our Privacy Policy.