To Safely Restart Elective Procedures, Look to the Data
This article is based on a 2020 Healthcare Analytics Summit (HAS 20 Virtual) breakout presentation by Nirav Patel, MD, Medical Director for Surgical and Procedural Services, Banner Health, and Martina Brooks, MHI, CSSBB, Surgical and Procedural Standardization Program Director, Banner Health, titled, “Effectively Restarting Elective Surgery After COVID-19.”
In March 2020, healthcare organizations across the U.S. suspended elective surgeries and procedures to reserve resources for patients with COVID-19. Though the delay in care has been a critical part of the COVID-19 response, it has resulted in significant revenue loss. The American Hospital Association estimates that four months of halted elective procedures have led to $202.6 billion in losses for U.S. hospitals and health systems, an average of $50.7 billion per month. Some experts estimate that the pause in elective surgeries has led to the biggest financial hurdle the healthcare industry has faced in years because these procedures are a primary income source for many health systems.
Facing financial strain (and even collapse), health systems welcomed the opportunity to resume elective procedures later in the spring of 2020—critical to financial recovery and sustainability—if they met CMS’s recommended criteria by state. However, the green light for health systems to restart elective procedures has highlighted a lack of data infrastructure and analytics tools to support an effective reactivation plan. To overcome this data and analytics barrier, work towards recovery, and prevent more lost revenue, organizations need a data-informed roadmap and analytics tools, including data visualization dashboards and predictive models.
Robust Analytics: The First Step to Safely Restart Elective Procedures
To understand the full-scale consequences of COVID-19 and restart elective procedures, health systems must first have access to robust analytics (clinical, financial, and operational). Without comprehensive analytics, leaders only see one piece of the picture, such as the clinical data without operational and financial context. Instead, with comprehensive information, leaders can see all of the opportunities to optimize the reactivation plan, avoid wasting resources, and generate income.
Access to complete data sets in one comprehensive platform (e.g., the Health Catalyst Data Operating System (DOS™)) allows health systems to view all of the data, then select specific data aligned with their reactivation goals. This broad data access enables organizations to measure progress and ensure they are on track to meet their procedural volume goals.
For example, if a health system wants to understand procedural case volume and canceled cases to inform the elective procedures reactivation plan, it needs access to analytics reflecting canceled cases, cancelation reasons, and completed cases with case completion details. Ideally, all members of the team, including providers, administrators, and other leaders, can access the same data and leverage the same information to drive decision making.
Data and Analytics Tools Drive an Effective Elective Procedure Reactivation Plan
Once the clinical, operational, and financial data is accessible in one place, a health system can focus on creating the data and analytics tools (e.g., data dashboards) to direct the reactivation process from the start. When health systems stopped elective surgeries, many relied on their existing data tools (typically delayed, manually-configured reports based on available data) to identify opportunities and inform a reactivation plan. However, without more effective data and analytics tools in place, leaders couldn’t quickly review real-time data to understand clinical resources, staffing, and supplies (e.g., personal protective equipment (PPE) and ventilators).
Effective information-sharing tools, such as data displays or dashboards (Figure 1), allow leaders to maximize data by seeing high-level information in a format that calls attention to outliers or trends. Building dashboards that can dynamically reflect new data also allows support staff to avoid scrambling to build one-off dashboards on partial data sets. With data and analytic tools in place, health systems are prepared to restart elective procedures as soon as they meet the CMS guidelines.
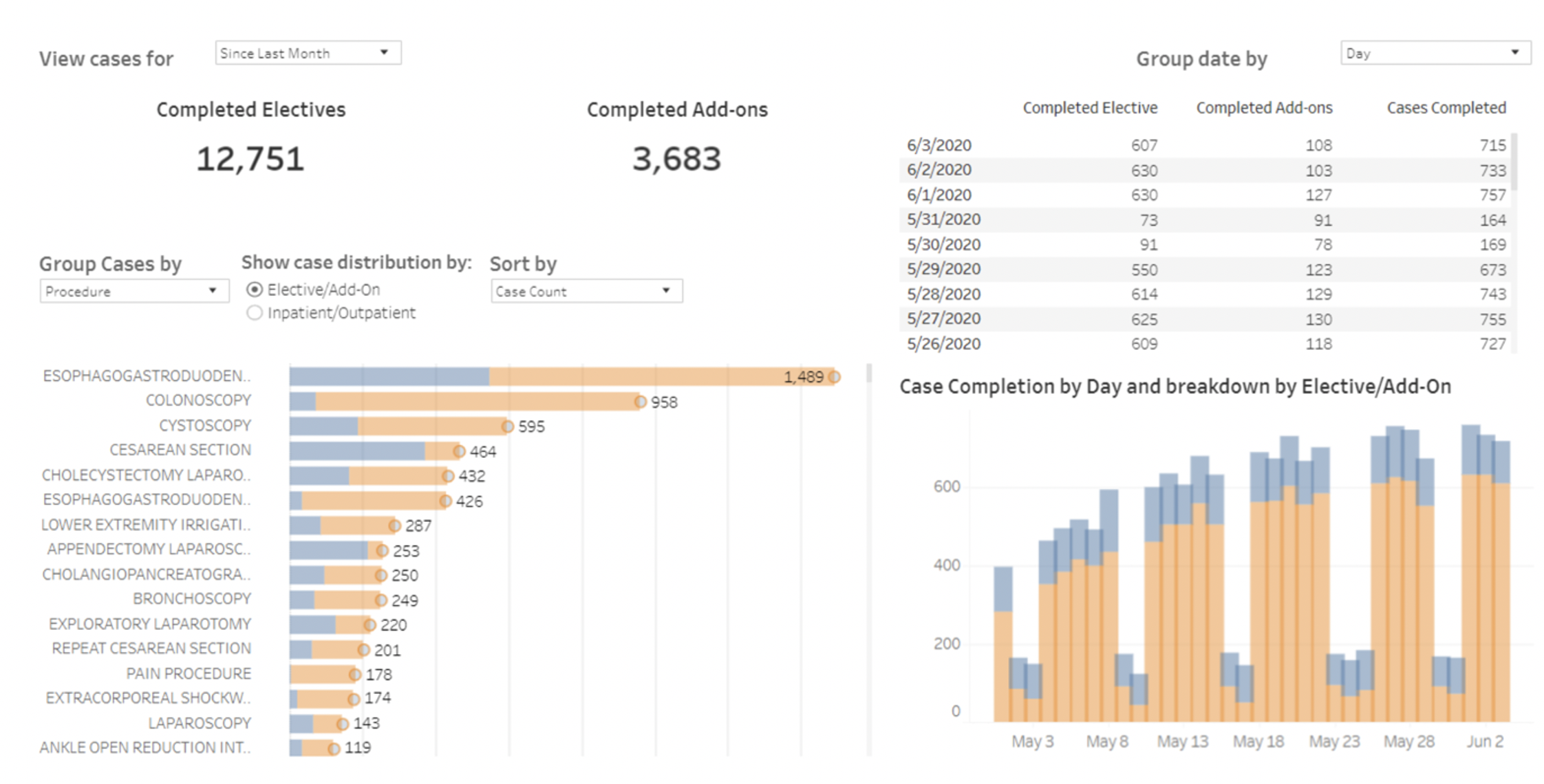
Another important piece of creating effective analytics tools is to include stakeholders from a variety of departments in the development process. Hearing different viewpoints about which data sets to include leads to a more comprehensive reactivation strategy. Systemwide access to the dashboards combined with the data visualization tools are also an opportunity for leaders to promote data-driven decision making and data sharing throughout the organization.
Predictive Modeling Promotes Flexible Approach to Restart Elective Procedures
Once health systems have created dashboards and given team members access to them, data experts can take the data one step further with predictive models. For example, capacity planning teams can add value to the reactivation process by helping health systems understand how many elective procedures they can accommodate relative to their clinical staff and supply resources. While predictive models can’t accurately forecast what will happen over the next six months because of the rapidly changing coronavirus, they can help health systems prepare for the next few weeks, a more effective approach than changing the strategy day by day.
With data-driven tools in place, data experts can create predictive models that provide insight into possible outcomes and responses. For example, if X happens, the health system should do Y. Or, if Y happens, the health system will do Z. Because COVID-19 is changing rapidly, directly impacting a health system’s capacity, predictive models can help organizations prepare for unexpected changes and support an adaptable reactivation response plan.
With predictive models informing decisions, health systems can create other actionable tools, such as a resource capacity model that incorporates information about staffing, hospital resources, length of stay, ICU, PPE, and ventilators. Data science teams can leverage the predictive models to measure the elective procedure volume a health system can safely accommodate. Based on the predicted volume from the model (taking into account historical and current volume data), the health system can develop criteria for which elective procedures to restart—rather than open at full capacity and risk shutting down due to a COVID-19 outbreak or capacity strains.
Data Fosters Sustainable Approach to Elective Procedure Reactivation Strategy
While health systems must plan to operate with COVID-19 for the foreseeable future, they can safely restart elective procedures with a data-informed reactivation plan. Comprehensive dashboards and predictive models offer visibility into various aspects of hospital capacity that impact elective surgery restart, allowing health systems to adjust resources to tactically resume these procedures.
Data and analytic insight allow leaders to compare historical information with current circumstances, revealing insights into filling gaps, future case volume, and resource utilization. These insights prioritize provider and patient safety, helping organizations get on the road to financial recovery.
Additional Reading
Would you like to learn more about this topic? Here are some articles we suggest:
- How to Optimize the Healthcare Revenue Cycle with Improved Patient Access
- Healthcare Relief Funding: Five Steps to Maximize COVID-19 Dollars
- Healthcare Revenue Cycle: Five Keys to Financial Sustainability
- Four Strategies Drive High-Value Healthcare Analytics for COVID-19 Recovery
- Reduce Bad Debt: Four Tactics to Limit Exposure During COVID-19
PowerPoint Slides
Would you like to use or share these concepts? Download the presentation highlighting the key main points.
Click Here to Download the Slides
This website stores data such as cookies to enable essential site functionality, as well as marketing, personalization, and analytics. By remaining on this website you indicate your consent. For more information please visit our Privacy Policy.

